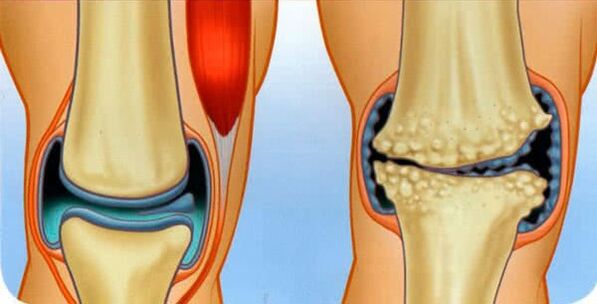
The surfaces of the bones that form the joint are covered with a special hyaline - smooth cartilage, which provides the minimum frictional force during the motor skills of the joint surfaces. If osteoarthritis is diagnosed, it means that the cartilage is being destroyed.
As the destructive process progresses it spreads to the bones and then to the joint capsule.
The disease has a universal microbial code 10 - M15-M19, classifying it as a class of pathologies of musculoskeletal and connective tissues.
According to medical statistics, 12% of the world's population suffers from osteoarthritis, most of which are elderly people aged 65 and over. However, every year there is an alarming trend towards an increase in the number of cases among young people.
The diagnosis is not fatal, but osteoarthritis is insidious with its relapses and the threat of complete disability.
Mechanism of origin
The disease develops gradually, we can conditionally distinguish four stages:
- Initially, an area of the cartilage that is poorly supplied with blood or damaged appears at the site of the cartilage. Gradually, in the presence of traumatic factors, the area is not restored, but, on the contrary, grows.
- The body, trying to restore collapsed cartilage, replaces the damaged areas with a mineralized tissue that does not have a clear structure. Such tissue is, in general, an inferior substitute for smooth, sliding and elastic hyaline cartilage.
- Gradually, the surface of the cartilage becomes covered with scars and bone growths - osteophytes.
- Healthy areas due to the increased load several times wear out very quickly, and as a result, the entire cartilage tissue turns into a large scar.
If the pathological process is not stopped, the joint will undergo the following adverse changes:
- bones are involved in the process of destruction;
- the synovial membrane becomes inflamed;
- the joint capsule becomes denser, losing its elasticity;
- the lumen of the joint space decreases rapidly;
- the bones, unable to resist friction, are deformed, as are the joint as a whole;
- the tissues of the joint are reborn, so there is a complete loss of the possibility of movement.
Types of osteoarthritis
This disease affects absolutely any joint surface! At the same time, despite the same pathology mechanism, it is classified into several types.
So, depending on which joints are diseased, they distinguish:
- osteoarthritis of the knee joint or patellofemoral arthrosis (abbreviated to gonarthrosis);
- osteoarthritis of the hip joint (abbreviated as coxarthrosis);
- arthrosis of the shoulder joint;
- interphalangeal arthrosis;
- arthrosis of the ankle joint;
- arthrosis of the hands;
- cervical arthrosis;
- arthrosis of the jaw;
- arthrosis of the metatarsophalangeal joint;
- arthrosis of the ileum;
- clavicular-acromial arthrosis;
- temporal arthrosis;
- arthrosis of the heels;
- arcuate arthrosis affecting the arcuate processes of the vertebrae (abbreviated to spondyloarthrosis);
- arthrosis of the joint of the facets of the joints of the spine;
- non-vertebral arthrosis;
- costovertebral arthrosis;
- talonavicular arthrosis.
According to the specifics of the course of the pathological process in the cartilage tissue, there are:
- deforming osteoarthritis is the name of a disease that has passed to the terminal (final) stage;
- arthrosis, - the presence of a classic inflammatory process is characteristic;
- chronic;
- acute osteoarthritis.
According to the causes of the pathology, there are:
- dystrophic arthrosis of the joints associated with a critical metabolic disorder;
- osteoarthritis of the fracture, caused by the corresponding injuries;
- post traumatic arthrosis.
It is important to know! There is no arthrosis of internal organs, for example, osteoarthritis of the heart is not a type of disease, but a consequence - a violation of heart activity due to the destruction of the cartilage of the thoracic region.
There is another classification, depending on whether the disease is independent or caused by provoking factors:
- primary - occurs on completely healthy cartilage, another name - idiopathic osteoarthritis or appears with age-related senile changes;
- secondary - caused by many reasons.
Symptoms of osteoarthritis
There are quite typical signs of arthrosis of all localizations, which, depending on the degree of development of the pathology, differ in their severity:
- aches, pain syndrome, aggravated by high humidity and hypothermia;
- reduced mobility of the joint;
- crackling, creaking and scraping sounds during movements of the joint surfaces;
- external changes in the profile of the joint;
- swelling and swelling;
- redness of the skin.
ache
The earliest signs of ailments are manifested by mild or moderate pain, of short duration, which almost never occurs at night, but usually appears only with a load on the joint surface.
When the inflammatory processes have passed to their final stage, the patient begins to feel an unbearable, "gnawing" pain due to the stagnation of blood and the increase in pressure in the joint bag. The pain is characterized by a long duration, at any time of the day, and regardless of whether the affected area is at rest or in motion.
joint stiffness
This symptom is typical of a fairly advanced disease. At the same time, in the early stages, the patient still feels in the morning, after waking up, discomfort when moving in the form of a feeling of stiffness.
As the destructive reactions progress, the patient notes:
- limitation of the amplitude of habitual movements;
- the inability to change the position of the limbs at rest, even when trying to manually stretch the joint;
- strong fixation (contracture) in a certain position of the joint, which for a long time was in a state of lack of motor activity.
Eventually, at the fourth stage of the pathology, ankylosis is formed in the form of replacement of joint tissues with scars, with a complete loss of functionality.
Sounds in the joint
A crunch can be accompanied by any bone and cartilage dysfunction, not just caused by osteoarthritis.
However, it is characteristic of this disease that the sound:
- occurs only in the joint that hurts;
- accompanied by difficulty in movement;
- it tends to intensify as the pathology progresses, and enters during the formation of ankylosis.
Change in the appearance of the joint
Notable changes appear in the later stages. Thus, the axis of the affected limb is bent, and the joint region itself is disfigured: it grows in size, the shape changes ugly.
All this testifies to the irreversible destruction of the joint, within which a new tissue has formed, not having a specific structure.
If such a pathogenic process occurs in the knee, the load on the ankle and metatarsophalangeal joints will increase, which will damage them over time.
If the externally deformed part of the body is also swollen or swollen, this means inflammation of the synovial membrane, as a result of which synovial fluid accumulates in large quantities in the joint bag, causing severe pain.
Causes of osteoarthritis
Pathology can occur both in a single joint, and spread to several. This disease occurs less often at a young age - there is still enough vitality for the body to self-heal.
However, for all age groups, the causes of onset in the direction of exposure are:
- internal - some diseases, bad habits, unbalanced diet, etc. ;
- external, - accidents, professional factor.
Internal causes are factors that provoke a negative change in the joint in the form of inflammation of the joint. There are inflammations of various origins:
- infectious (E. coli and Koch's bacillus, viruses, chlamydia, staphylococci, Treponema pallidum, etc. );
- rheumatism;
- purulent arthritis;
- autoimmune nature;
- gout;
- psoriasis.
In addition, the causes of internal exposure include congenital or acquired disorders of the structure of the cartilage and malnutrition, which can be associated with:
- failures and genetic mutations;
- abnormalities of intrauterine development, including perinatal trauma;
- old age;
- osteoporosis, ie "washing" of the constituent elements from the bone tissue;
- hormonal disorders and overload, including menopause;
- violations of normal metabolism;
- nutritional deficiencies of vitamins and minerals;
- diseases that cause muscle weakness;
- prolonged internal intoxication.
The exacerbation of many diseases of the musculoskeletal skeleton also leads to the degeneration of the cartilage.
External causes of the development of the disease are factors that damage the joint, such as:
- frequent hypothermia;
- dislocations;
- strong blows;
- fractures;
- injury of the meniscus;
- strong physical activity (weight lifting, for example);
- professional sports;
- joint surgery.
Degrees of osteoarthritis
According to the clinical manifestations and the process of progression of the disease, four stages of osteoarthritis are distinguished:
- 1st degree arthrosis, this is the initial stage of arthrosis, characterized by hidden symptoms in the form of negative changes in the composition of the synovial fluid and weakening of muscle fibers, if pain appears, it is only during physical exertion;
- 2nd degree arthrosis - this is already a pain sensation due to the collapse of the bone joint and the formation of osteophytes, the reflex neurotrophic regulation is disturbed and an audible crunch appears;
- 3rd degree arthrosis is characterized by significant degenerative changes in the joint, its visible deformation with a curvature of the axis of the limb, the ligaments shorten and the joint becomes pathologically mobile;
- 4th degree arthrosis is complete ankylosis, complete contracture and severe pain even at rest.
All four stages proceed unevenly: during the pathological period, sharp exacerbations and moments of remission are possible.
Treatment of arthrosis
It has been clinically proven that treatment and prevention in the form of elimination of the provoking factors of hyaline cartilage damage, although they do not alleviate the disease in the initial stage, stop its development and restore the functionality of the joint.
Basically, the disease of small and moderate severity is treated with conservative methods. In case of severe destruction of the cartilage surface, which has led to the destruction of the bones, surgical arthroplasty is indicated.
In this case, the cardinal principles of the treatment are:
- an integrated approach that involves the use of multiple therapeutic methods;
- intentionality, that is, the concentration of efforts on eliminating the factors and consequences that cause the disease.
Treatment with folk remedies
Being treated comprehensively, but at home, you can also resort to the healing recipes of traditional healers, offering effective treatment of health problems through herbs and bee products.
From plants use:
- bay leaf in the form of decoctions, specially prepared vodka tinctures and oils, used externally, directly on the inflammation zone;
- the treatment of arthrosis with honey has established itself as a reliable local drug that relieves inflammation in the form of rubbing and nourishes the skin, muscles and cartilage;
- cabbage leaf, - better than white cabbage, - knead it a little, wrap it around a sore spot, heat it with a woolen cloth on top and keep it overnight;
- aloe juice in the form of compresses and rubbing into the skin;
Treatment of arthrosis of the knee joint with burdock also helps: the leaf is bandaged on the sore spot, which is isolated for the whole night.
It is important to know! Using herbal medicine, it is necessary, to enhance the effect, to forget bad habits and take care of proper nutrition.
Medicines for osteoarthritis
Drug treatment related to the classical method of therapy is divided, depending on the dosage form used, into drugs:
- external use, in the form of an ointment for arthrosis, rubbing, lotions;
- injections;
- pills for osteoarthritis;
- capsules.
Ointments
The pharmaceutical industry produces medical ointments based on highly active natural ingredients:
- heparin ointment.
A remedy containing 1% diclofenac helps well - the gel is applied to the skin.
Injections
Injections have proven to be very effective in treatment, not only intravenously and intramuscularly, but also directly in the affected area, for example with non-steroidal drugs.
Then, intra-articular injections are injected into the damaged joint tissues:
- glucocorticoids, which improve the nutrition of cartilage tissue, relieve inflammation and increase elasticity;
- chondroprotectors and analogues of intra-articular fluid;
- hyaluronic acid as a lubricant and analgesic.
Preparations in the form of tablets and capsules
A special group in drug therapy are the so-called chondroprotectors for osteoarthritis, which contain the structural elements of hyaline cartilage and thereby restore it.
These drugs are available in the form of tablets and capsules intended to be taken orally via the gastrointestinal tract (orally).
Also, patients are prescribed NSAIDs - anti-inflammatory drugs for osteoarthritis of the non-steroidal group, which block acute pain and relieve exacerbations.
Pain relievers are also used in the form of novocaine blockade.
Also, complex vitamins are prescribed for osteoarthritis.
From natural preparations of local action, medical bile is recommended, applied in the form of compresses to the skin.
Exercises for osteoarthritis
Excellent special exercises and remedial gymnastics (LFK) have proven themselves, the complex of which provides physical activity on the diseased part of the body in a gentle and dosed way.
Dr Bubnovsky and Evdokimenko have developed their own sets of therapeutic exercises.
It is important to know! Physical exercises help very effectively to restore health, but only if it is used at the very beginning of the development of the disease!
Massage for osteoarthritis
A very beneficial effect on medical treatment and massage, which improves microcirculation and nutrition of deep tissues.
Diet for arthritis
In this condition, it is important to adhere to proper and rational nutrition in order to slightly improve the patient's condition. Abstinence from overeating, the exclusion of animal fats and fried foods is recommended.
It is important to know! In addition, in the fight for healthy cartilage, physiotherapy in the form of magnetotherapy, electrophoresis, paraffin and therapeutic mud packs should be used.
Which doctor treats arthritis
First of all, with complaints of pain in the joints of the bones, you should go to the therapist. It is he who, having summarized the history of the patient and having asked him in detail, will refer to the necessary narrow specialist.
It can be, depending on the cause of the disease and its type, doctors of profiles such as:
- orthopedic;
- traumatologist;
- surgeon;
- rheumatologist.



















